Frailty within the health system
Our current healthcare system is at a tipping point, where unprecedented levels of frailty in an aging population collide with a specialized healthcare system that was designed to address one problem at a time. The fragmentation of health issues into discipline-specific silos creates an inefficient and chaotic experience and doesn’t provide value for money. Currently, 50% of health expenditures occur during the final 6 months of life, yet there is no evidence that those expenditures create a better patient experience.
So, how do we move forward? In order to create a more responsive experience for those with complex health issues, the system must embrace the concept of frailty. Frailty exists when the accumulation of health issues over the lifespan starts to impair function, mobility, or cognition. Key features of frailty include:
- Although rarely recognized or measured in routine care, frailty is a key predictor of how a person will fare with standard of care interventions (regardless of age, intervention, or healthcare setting).
- Frailty is not the same as age. It’s more akin to a life stage that eventually affects all individuals who live long enough.
- Frailty progresses over time. Although many programs aim to delay or reverse frailty, much of frailty appears to be irreversible. In fact, in some ways, optimal chronic disease management creates frailty by increasing long term survival.
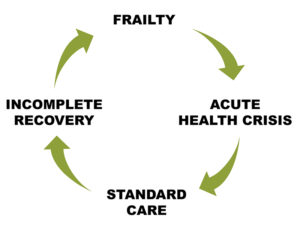
- The factors that contribute to frailty vary widely, but all individuals who are frail will have a health crisis (a sudden worsening of an existing health problem or the emergence of a new one). When standard care is applied, recovery is often incomplete and involves further frailty. This is called the frailty cycle.
The PATH model
Palliative and Therapeutic Harmonization (PATH) is an innovative, award-winning model, designed to improve the patient and family experience of frailty while optimizing resource utilization. The PATH model enables healthcare teams to understand and respond to frailty and empowers patients and families with information and skills to help them navigate each stage of frailty.
PATH’s clinical model uses proven tools and techniques to address frailty in 4 steps:
1 Understand
A standardized approach to understand the big picture of health
2 Communicate
Proven communication techniques to ensure a shared understanding of a person’s health story and prognosis
3 Empower
A framework for patients and families to make decisions in advance and learn skills to approach decisions that may be needed during a health crisis
4 Respond
Navigation and support at home during the health crisis or when major interventions are proposed
Why PATH works
For the health care system
- Streamlines, triages, and builds efficient care
- Provides a consistent approach to frailty across the health care continuum
- Identifies and responds to vulnerability
For health care professionals
- Fosters true collaboration with improved efficiency
- Increases provider appetite for change and desire to avoid poor patient outcomes
For patients and families
- Optimizes the patient and caregiver experience of care
- Provides clarity about the alternatives to aggressive care
- Supports patients and families during times of crisis
PATH represents a full systems solution to the challenge of frailty:
- Achieving more with less: PATH meets the Institute for Healthcare Improvement (IHI) Triple Aim Criteria. Application of the program improves clinical outcomes and the patient/caregiver experience, while significantly reducing per capita costs. PATH can often be implemented without the addition of net new human resources.
- Setting the standard: PATH has been recognized as a Leading Practice by Accreditation Canada.
- Developing the evidence: PATH is at the leading edge of evidence-informed best practices for appropriate care in frailty. We are committed to quality improvement through ongoing research and evaluation.
- Growing the solution: PATH has been adapted for implementation in multiple care settings across Canada, including primary care, acute care, pre-operative care, nephrology, cardiology, medical oncology, rehabilitation units, and long-term care.
- Aligning with deliverables: PATH is aligned with the strategic directions of the Nova Scotia Health Authority Frailty Strategy, the first provincial strategy to directly address frailty.
Our clients include:
- Healthcare teams
- Clinics that focus on a particular area of care (e.g., cardiology decision-making, pre-operative assessment, management of challenging behaviors in dementia, end stage renal disease, and oncology)
- Facilities interested in implementing the model as a new standard of care to manage frail patients (e.g., Assess and Restore, long term care, and academic/community hospitals)
- Health authorities and networks interested in achieving better outcomes and sustainability across the care continuum